Respiratory Disease Risk Increase
Climate change poses many risks to human health, including increased respiratory disease risk from exposure to allergens and harmful air pollutants. Research shows that climate change has led to longer pollen seasons, allowing for the production of more plant-based allergens, and more active wildfire seasons that increase human exposure to harmful smoke. Higher temperatures associated with climate change can also lead to an increase in ozone, a harmful air pollutant.
Read More



Climate science at a glance
- Warmer temperatures and longer seasons can lead to the production of more plant-based allergens that increase allergic sensitizations (the process by which the body becomes sensitive and allergic to a particular substance) and asthma episodes.[1][2][3]
- Scientists have identified the fingerprint of climate change on lengthening pollen seasons and increased allergic disease burden in the United States.[4][11]
- By increasing wildfire activity, climate change increases human exposure to harmful smoke.[5]
Background information
What is pollen?
Pollen is a powdery substance that is released into the air by plants, such as grasses, weeds, and trees. Pollen grains float through the air – if they land on another plant of the same species, they can fertilize it to produce seeds for a new plant. Plants only release pollen into the air throughout the warm “pollen season”. For the US, this begins – depending on the state – around February and continues throughout the summer.
How does climate change affect pollen season and associated health risks?
Pollen is one of the most common triggers of seasonal allergies, and research shows warmer temperatures and longer seasons due to climate change increase the health risks associated with pollen.[1][2][3]
How does climate change affect wildfire smoke and associated health risks?
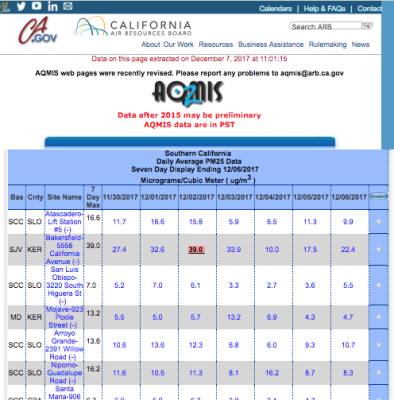
Smoke from wildfires contains large abundances of fine airborne particulate matter (PM2.5), known to cause a variety of short and long-term health problems, with the clearest evidence for exacerbations of asthma and chronic obstructive pulmonary disease. Climate change has increased the frequency, intensity and spread of wildfires, especially in the western US. The increase in wildfire activity has been accompanied by substantial increases in the number of days with any smoke in the air across the United States.[5]
US trends related to increased respiratory disease risk and climate change
- (Burke et al. 2021): The contribution of wildfire smoke to PM2.5 concentrations in the US has grown substantially since the mid 2000s, and in recent years has accounted for up to half of the overall PM2.5 exposure in western regions as compared to <20% from 2005-2010.[5]
- (Schnell et al. 2017): The weather factors that drive heat waves also contribute to intensified surface ozone and air pollution episodes. These extreme, multiday events tend to cluster and overlap, worsening the health impacts beyond the sum of their individual effects.[6]
- (Tong et al. 2017): There was a 240% increase in the number of large dust storms between the 1990s and 2000s.[7] Large-scale variations of sea surface temperature in the Pacific Ocean are likely behind this trend. In the Southwest, the infection rate of Valley fever has mysteriously gone up more than 800% from 2000 to 2011. In two endemic centers, dust storms are found to be better correlated with the disease than any other known controlling factor.[7]
- (Wang et al. 2016): There is a causal link between PM2.5 (fine particulate matter with a diameter <2.5 microns that comes from vehicle exhaust and other sources) and all natural-cause mortality in New Jersey from 2004 to 2009.[8]
- (Ziska et al. 2011): The significant increase in the length of the ragweed pollen season — by as much as 13–27 days at latitudes above ~44°N in North America since 1995 — was associated primarily with a delay in first frost of the fall season and lengthening of the frost-free period.[9]
US studies attribute increases in respiratory disease risk to climate change
- (Anderegg et al. 2021): Pollen trends across North America from 1990 to 2018 reveal an increase in pollen concentrations and longer pollen seasons, and climate change is the dominant drive of the change.[4]
- (Sapkota et al. 2019): Climate change-driven ecological changes are directly linked to allergic disease burden in the United States.[11]
Global trends related to increased respiratory disease risk and climate change
- (Ziska et al. 2019): There is a clear positive correlation between recent global warming and an increase in the seasonal duration and amount of pollen for multiple allergenic plant species on a decadal basis for the northern hemisphere.[10]